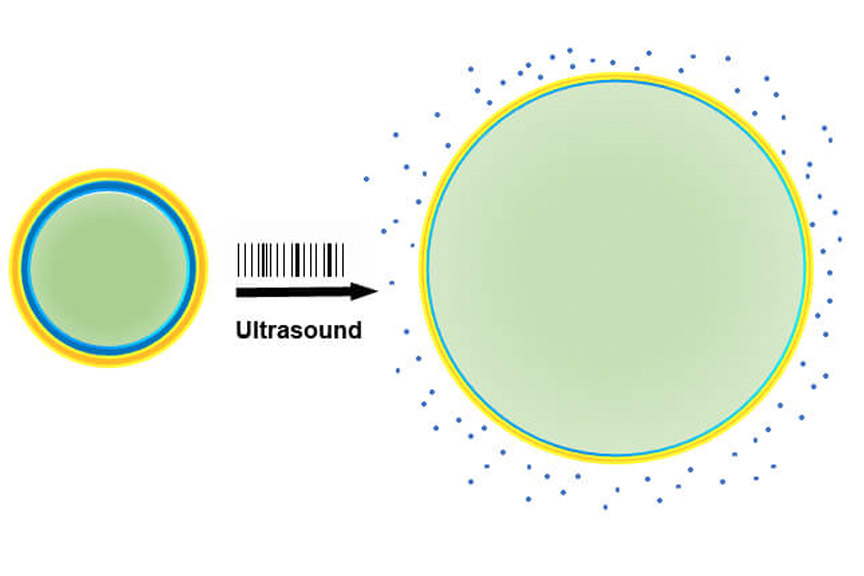
JOHNS HOPKINS RESEARCHERS REPORT THAT A NEW PEPTIDE HOLDS PROMISE FOR IMPROVING TREATMENT FOR DEGENERATIVE RETINAL DISEASES, SUCH AS AGE-RELATED MACULAR DEGENERATION, DIABETIC MACULAR EDEMA AND DIABETIC RETINOPATHY. THESE VASCULAR DISEASES OFTEN RESULT IN CENTRAL VISION LOSS AS BLOOD VESSELS GROW INTO TISSUES AT THE BACK OF THE EYE, WHERE SUCH GROWTH SHOULD NOT OCCUR.
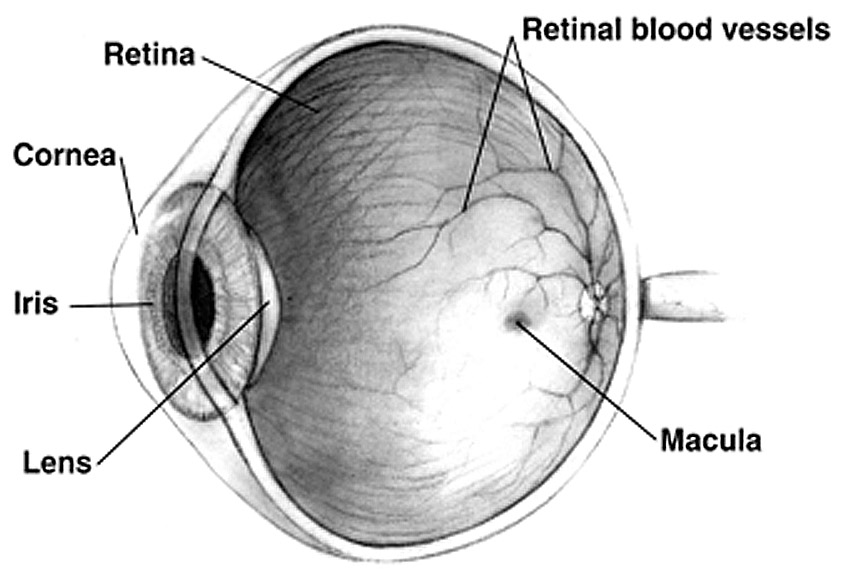
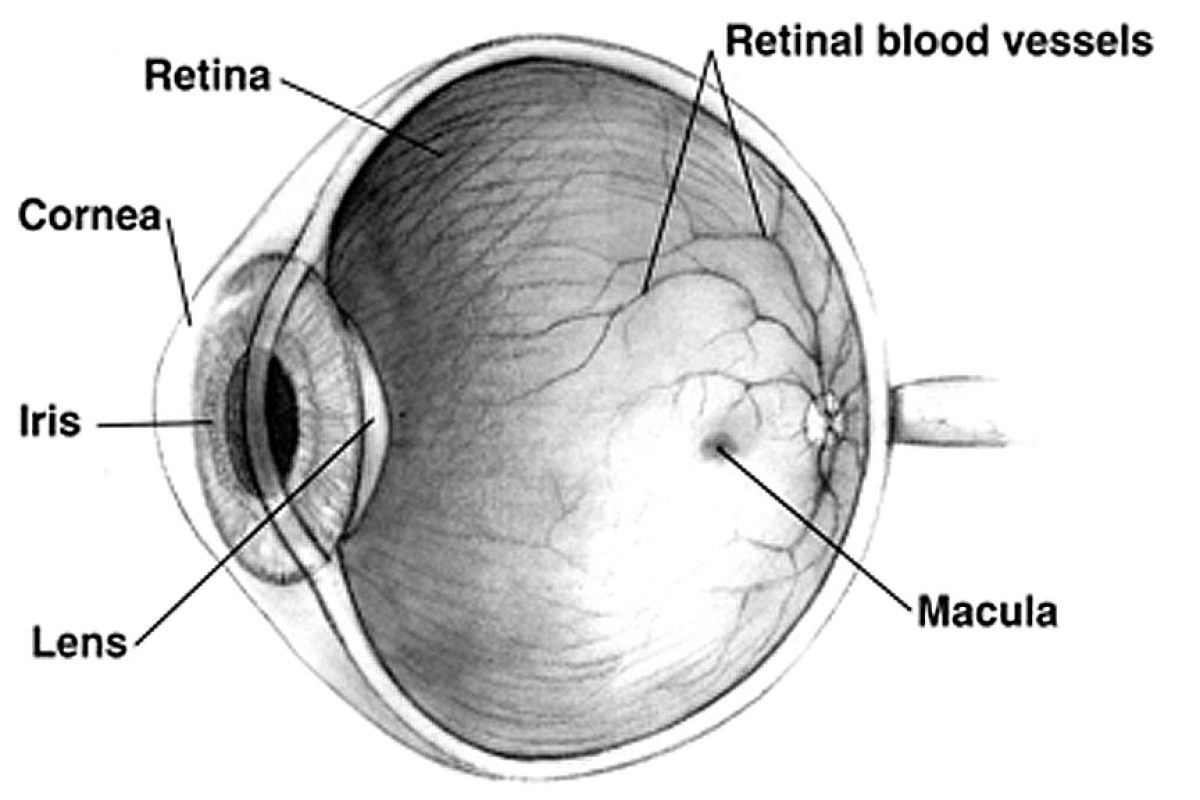
Cross Sectional Eye Anatomy. Credit: NIH National Eye Institute
The study, published Jan. 18 in Science Translational Medicine, shows that the injectable peptide may more strongly suppress abnormal blood vessel growth and leakage in the eye, cause regression of established abnormal vessels, and may last longer when compared to current treatments. If proven effective in humans, this could mean that patients need only a few needle injections to the eye per year, instead of the monthly injections that are the current standard of care.